Ever since early humans first tasted alcohol from fermented fruit, people have been fascinated by drugs that affect our conscious state, whether that is by making us drowsy or by causing hallucinations. From caffeine to cannabis, we now have a vast array of these drugs, but scientists still don’t fully understand a class of consciousness-altering drugs that is crucial to modern medicine: general anaesthetics.
There is no comparison between surgery now that we have general anaesthetics and the horrific reality of surgery in the past. The invaluable contribution of general anaesthetics to medicine has motivated a lot of research into their properties, but finding out how they work is proving to be a challenge. A major source of confusion is that they have very little in common with each other structurally and therefore chemically (illustrated below), yet it seems unlikely that a group of molecules that elicit the same response wouldn’t have characteristics in common to cause that response. Scientists have embraced this puzzle and spent many years trying to decipher what’s going on.
One of the first theories for anaesthetic action came from experiments done by German pharmacologist Hans Horst Meyer and British physiologist Ernest Overton. They proposed that anaesthetics dissolve in the fat that surrounds each cell, making it difficult for nerve cells in the brain to communicate with each other. Meyer and Overton’s evidence for this was their discovery of a correlation between the degree to which various anaesthetics can dissolve in fat and how potent they are. This theory was useful because it suggested a common physical property of anaesthetics, which removed the problem arising from the large variety of chemical properties and molecular structures that makes anaesthetics so baffling.
However, it later became apparent that the dissolving of anaesthetics couldn’t possibly fully account for how they worked. The most obvious problems for the theory were the exceptions to the correlation; molecules with an identical ability to dissolve in fat but different anaesthetic potencies were identified. At the very least that means the ability to dissolve in a cell membrane cannot be the whole picture for anaesthetising power. Over the years, other observations were made that threw further doubt over theories solely based on the dissolving of anaesthetics.
In the 1980s and ‘90s, a number of major breakthroughs were made, owing to the development of genetic engineering and imaging techniques. One of these was the discovery that many anaesthetics bind to a type of receptor on nerve cells that responds to the presence of GABA (a chemical produced in the brain) by reducing communication between neurons. When anaesthetics bind to GABA receptors, they artificially make neurons more sensitive to the effects of GABA, thus reducing neuron communication (as illustrated in the diagram). The lack of structural similarity between different anaesthetics is accounted for in this theory as anaesthetics bind to different places on the receptor, so a common shape to fit one site isn’t needed.
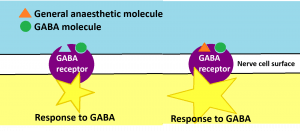
This discovery fits with other consciousness research, as it’s thought that communication between different brain regions is responsible for bringing about conscious awareness. The evidence for this is that when a person is unconscious, information still reaches some parts of their brain but is not sent to other areas for processing, whereas in a conscious person there is a high level of communication between brain regions. If anaesthetics tamper with GABA receptors, their ability to cause a loss of consciousness would make sense because GABA reduces the communication between neurons.
What seems most probable is that anaesthetics interact with specific proteins on the cell surface rather than affecting the whole surface by interfering with its fatty foundations as previously thought. However, it’s unlikely that this is the full story. In the current model, the fact that so many anaesthetics dissolve easily in the fat of cells is given little significance. As well as this, some anaesthetics have been shown to bind to different proteins on the cell membrane, which revives the old puzzle of why drugs with such similar effects have such different mechanisms. Recently, scientists have started to propose theories >that combine the physical properties of anaesthetics with their chemical ones, but at the moment these theories require more research before they’re fully comprehensive.
Though anaesthetics aren’t shrouded in mystery as they were once were, we’re still a way off being certain of how they work. The theories described above are just a snapshot of anaesthesia research – scientists are still investigating new possibilities of how anaesthetics might interact with nerve cells. Hopefully in the future, our growing knowledge will lead to the production of new, more effective anaesthetics or a greater insight into human consciousness. In the meantime, the research certainly provides food for thought.

